Monthly Archives: October, 2011
CULTURAL COMPETENCY: MORE THAN A CHECKLIST
Posted: October 18th, 2011
When I arrived at our MCH program’s cultural competency training. I didn’t quite know what to expect. In the program description there were terms that piqued my interest such as “ghost busting”, “time spirits” and “cultural transformation”. It seemed quite hyperbolic to describe a training to increase organizational effectiveness. But, one of my core values in the workplace is the well-being of all, so I felt like this would be an applicable training for me to attend.
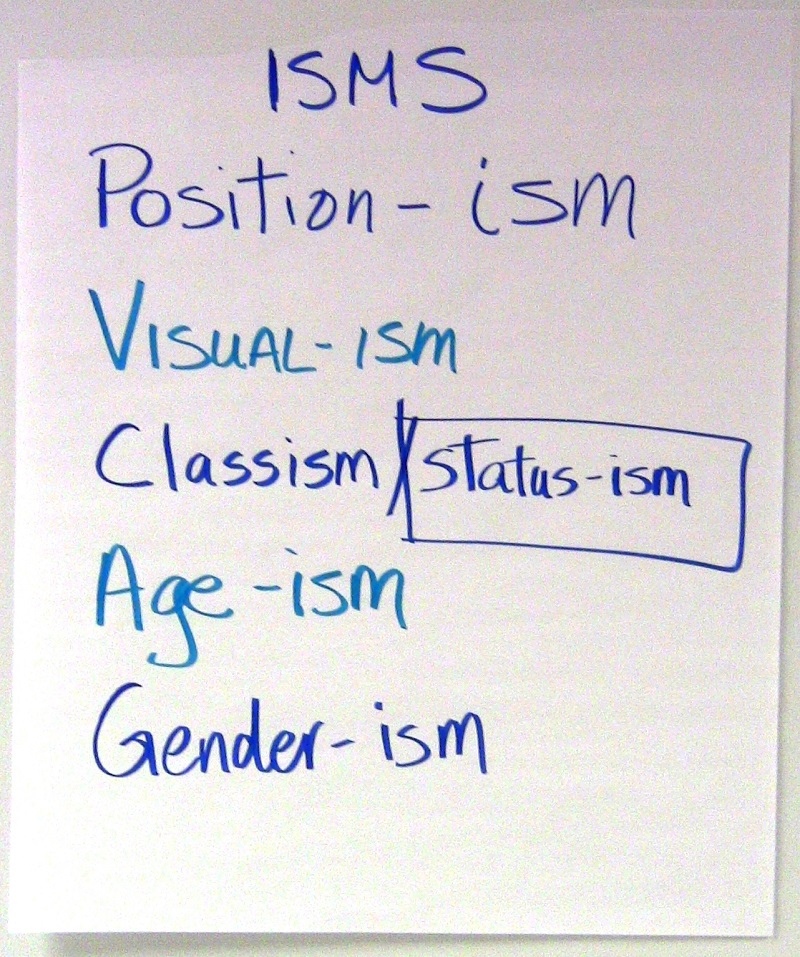
The chairs were set in a U-shape. There were two chairs at the front. A large screen was there, but no projector equipment. I thought there would surely be some IT professionals arriving soon, because is there a such thing as a training with no PowerPoint? After having breakfast, Grace Flannery and Marita Fridjhon, our facilitators, briefly described our agenda for the day. We were to describe various “-isms” that we encountered in the workplace (both the ones that we project and the ones that we receive), in the morning session, and in the afternoon, we would come up with strategies in which we could address these –isms. It seemed relatively simple to me, but where were the bulletpoints, pictures, and lists that almost always accompany such trainings?
There were none. Grace and Marita used simple large post-its displayed on easels. We did have a program booklet to accompany the program, but it was mostly used as a reference to some key points. The purpose of the booklet was mostly to jot down some notes and to have something to refer to once the training was over. The 30 of us engaged in conversations, shared experiences, and challenged our own thought processes. The facilitators led us through a wide variety of moods; happiness, sadness, empathy, joy, pensiveness, to name a few. In the end, we learned that as a seemingly heterogeneous group, more of us were alike than we were different. We were armed with the tools we needed to personally influence those around us, by making an attempt to understand their background, before making judgments and thus having non-productive interactions with them. While it seemed to be a bit ambitious goal at first, I’ve truly become culturally transformed.
**NOTE: We invite other attendees to share their stories.**
Written by: Bekeela Watson, UIC MCH, Graduate Education Coordinator
Photo: Bekeela Watson and Kris Risley, DrPH, CPCC, MCHP Continuing Education Director & Clinical Assistant Professor (right to left)
TIME SPIRITS AND CULTURAL TRANSFORMATION

Posted: October 18th, 2011
On Friday, October 14, 2011 the UIC MCH Program in collaboration with the UIC LEND program, the Mid-America Public Health Training Center (MAPHTC), and the Wisconsin Pediatric Pulmonary Center (UW PPC) sponsored a day-long Cultural Diversity training at the UIC School of Public Health. Typically, I do not participate in events that I am involved in planning; however, I did have the time to participate in this one. I learned more about how Time Spirits are shared cultural constructs/beliefs that we share from any era of history and that continue to have an impact on us and our society (ie, slavery, Jim Crow laws, women’s experience of not being allowed to vote/own property/work outside the home, etc.). I learned that -isms (racism, ageism, genderism, and some other -isms that we created words for [positionism, visualism]) are fueled by Time Spirits!
During this training, the 30 diverse participants explored four -isms (positionism, visualism, ageism, and genderism) and discussed how others discriminate against us using these forms of -isms and the impact this has on us both personally and professionally. I was in the visualism group with many others of different races/ethnicities and it was so interesting to be part of this small, diverse group sharing this common form of discrimination. We talked about how just showing up invites people to discriminate against us (or at the very least try to make up all kinds of stuff about us simply by how we look and how this becomes a self-fulfilling prophecy of sorts). I’ve been dealing with this most of my life so I know there is quite a bit of healing for me to do in this area. I was grateful to have the opportunity to realize just how painful this has been for me and to experience in a new way the tremendous impact this has had on me and my life path!
We then spent some time looking at the ways in which we individually discriminate against others – not an easy discussion! This was another huge learning opportunity which gave me the chance to re-think how I want to show up in the world! Again, so grateful for the learning. Personally, this gives me a stronger foundation of understanding and more courage to do what has been in my heart for a long time!
time continued
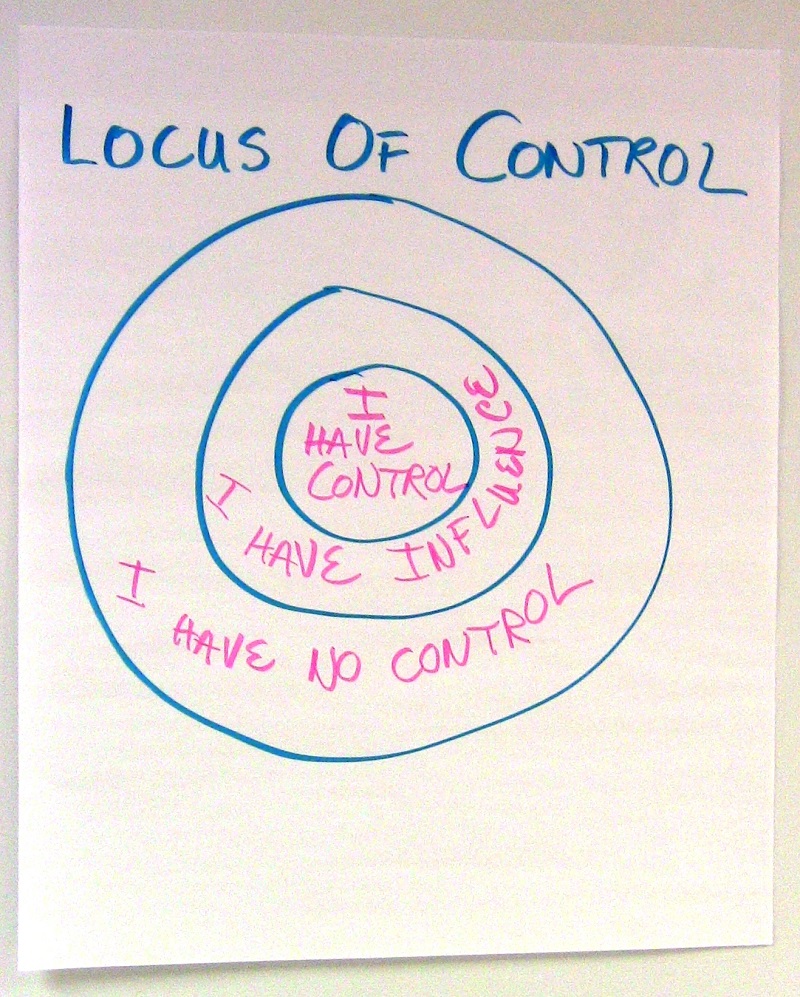
Finally, we explored our ‘locus of control’ or where we might be able to use this work to influence our own behaviors and work and interactions and where we might have some sort of positive influence. We also discussed where it was probably going to be impossible to have any influence. My take-away message is that I will work where I can have some influence and trust that these baby steps are impacting systems but that it will take time to see systems-level changes (even though I trust they are happening)! And, by the end of the day, I reconnected with old School of Public Health Colleagues and new colleagues to start a grass-roots effort to impact the culture in our own School of Public Health. This was an unexpected outcoome! All-in-all, a very productive, healing, and hopeful day!
**NOTE: We invite other attendees to share their stories.**
Written by: Kris Risley, DrPH, CPCC, MCHP Continuing Education Director & Clinical Assistant Professor
Photo: Bekeela Watson, MPH , MCHP Graduate Education Coordinator and Kris Risley (right to left)
JANUARY 2012 UIC MCH LEADERSHIP DEVELOPMENT AND COACHING PROGRAM
Posted: October 10th, 2011
The UIC MCH Program is currently accepting applications for the UIC MCH Leadership Development and Coaching Program which will begin in January 2012. This is a 6-month, distance-based program that includes 6-monthly, 1-hour calls focused on Authentic Leadership Development: Strengths Based Leadership, Values-Based Leadership and Decision-Making, Self-Awareness, Emotional-Intelligence, Ideal-Self, Work-Life Balance, Self-Care, and Whole Life Leadership. Each participant also meets with a personally assigned, certified, professional coach in two, 45-minute phone sessions every month. Additionally, participants identify a set of unique goals s/he will work towards over the course of the program. For additional information, please visit our website and/or review the attached January 2012 Program Description and Application. A limited number of scholarships are available for Family Leaders in MCH.
Applications are due November 14. Individuals will be notified about program acceptance by November 30. If you have questions, please contact Jaime Klaus at jaimkl@uic.edu or Kris Risley at kyrisley@uic.edu.
2011 PRACTICUM EXPERIENCES

Posted: October 4th, 2011
My Journey through India and Bangladesh
On my fifteen hour plane ride to India this summer, I reviewed numerous articles about menstrual regulation, abortion and mid-level health providers in Bangladesh and around the world. Menstrual regulation is legal in Bangladesh and is used to empty the uterus when a woman’s menses has been delayed up to 10 weeks. It is done before a pregnancy test or ultrasound has confirmed that the woman is actually pregnant and results in her resuming her menses. In reading all of these articles, I was preparing for a 5-week trip to India and Bangladesh where I would have the opportunity to do my field experience by working with the International Planned Parenthood Federation (IPPF). During my practicum, I was based in India with the South Asia Regional Office of IPPF. I worked with the dedicated abortion team to design clinical guidelines for the management of incomplete abortion and its associated complications.
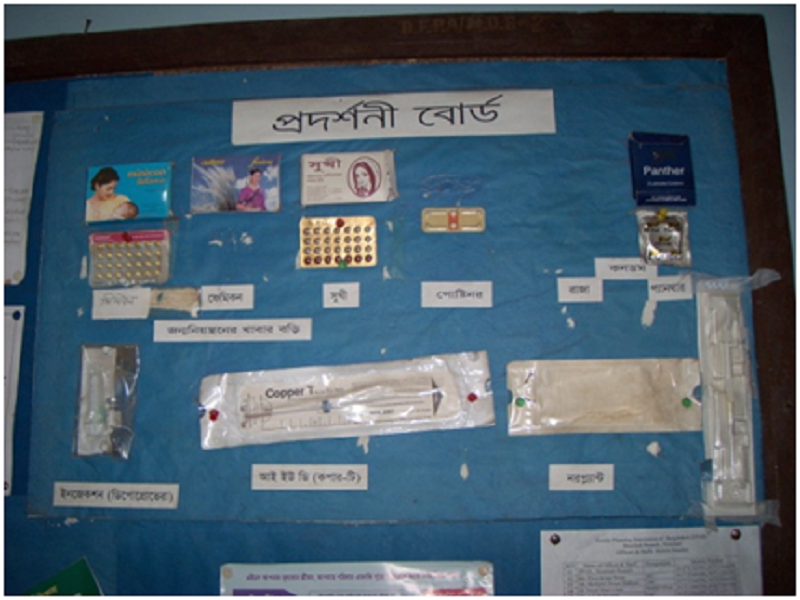
Once I had gained an understanding of the reproductive health care needs of women in Bangladesh and the availability of services, I was able to construct the clinical guidelines within the context of the resources and policies of Bangladesh. Thus, the practicum enabled me to do policy work, which is an area that I often do not get to spend time on in my daily work in the United States. Once these guidelines were complete, we traveled to Bangladesh to introduce and review the guidelines with key stakeholders in the reproductive health community of Bangladesh. We then held a conference for mid-level providers, which were the women who actually provide reproductive health care services within Bangladesh. From this conference, we were able to provide training about menstrual regulation, updates on contraceptive methods available, and a supportive community for the women to truly be heard.
practicum continued
This field experience was an incredible opportunity to learn about reproductive health with a hands-on approach in a setting completely different from my work as a Family Planning Fellow in Chicago. In the future, I plan to work with IPPF to continue to address reproductive health needs of women around the world. Seeing this experience through a public health lens has enabled me to gain a greater understanding of the needs and resources that impact communities around the world and the impact that family planning can have on women and their community.
by Tara Kumaraswami, 2nd Year MCH-MPH Student, Family Planning Fellow
The Trials of Public Health Work in a New Cultural Experience

Sarah Kammerer spent the summer interning for a small Indian-run NGO called Ekjut, located in a rural town in the eastern state of Jharkhand. She spent the summer developing an intervention that addresses family planning and contraceptive use within the marginalized tribal communities that Ekjut serves.
Here is a glimpse of one of her journal entries, while in India.
The most common question I’ve received since arriving in India is “What’s it like?”
I’ll start with the easy stuff.
It’s about 2 kilometers from my flat to the office. I’m picked up and dropped off each day by one of my coworkers on their motorcycles. The roads are terrible. Animals are everywhere. No building or store remotely resembles anything from home. Food stands are set up along the road, but no grocery store for a hundred miles. Once you pass through town, you are immediately transported to a scene from the Jungle Book: rice patties, mist covered mountains and elephants.
But the people? They are the same. Adults go to work, kids go to school. Women stand outside their houses in the evening and gossip about the latest news in the town. Men tinker on their motorcycles or relax over a beer (the local tribal beer is known as Handia). But instead of women in high heels and shoulder bags, they walk barefoot with large baskets on their heads filled with laundry or food or rocks. Small children entertain themselves with rocks and sticks, not Barbies and Tonka trucks. Girls, in their deep purple and lavender school uniforms and pigtails, ride to school not on big yellow buses, but government provided bicycles.
These are the things that are easy to get used to. It’s everything else that’s hard.
The other day as I was riding to work, there was a woman passed out on the side of the road, her sari around her waist, exposing everything for the world to see. I do not know what was wrong, she could have passed out from the heat or perhaps from something else. I asked my friend if we should stop, but he said we needed to keep going, her family would probably be there soon. Nearly a week later, I still think of her, I still cry for her. I wish I could have done something. I can throw out all the excuses in the world: I can’t speak Hindi, much less any of the tribal languages in the area, I’m not a doctor, I wasn’t about to jump off a moving motorcycle, but none of them make me feel better: a woman was helpless on the side of the road and I didn’t stop to help. What happened to her, I will never know, but I do know I will never let it happen again.
And it’s not just the images, it’s the stories too.
One woman delivered in the hospital, was released immediately after giving birth, only to hemorrhage as she was practically shoved out the door. She died in front of the hospital.
An Ekjut facilitator from a local village shadowed a nurse at the hospital for a week. Understaffed, she was immediately put to work. The nurse told her to rinse off the dirty needles and put them in a box to be “reused when the nurses make their rounds in the villages.” Imagine how you would feel if learning that your own friends and family didn’t even deserve clean needles.
Or what about reports from the village women, who upon arriving at the hospital are turned away. Why? Because maybe the doctor didn’t show up that day or maybe he was just too busy to take another patient. And if the women actually are admitted, they are treated with such disrespect; they vow never to return again.
trails continued

The worst part? These stories are a dime a dozen. But, that’s why I am here, right? To learn about Ekjut and what makes them successful, to do research about a subject that I love and ultimately, work for the improvement of maternal health in underserved, marginalized communities.
So, India? It’s a crazy, beautiful place. At times it’s mind-boggling, heart-wrenching and absolutely exhausting. But it’s becoming home and without a doubt, everyone at Ekjut is family.
Overall from this experience, Sarah learned about Ekjut’s vision and how they turned it into reality. She learned more about Ekjut’s methods, their strength, and weaknesses. She also learned how to put together a project proposal and develop an intervention program, while also gaining knowledge of Indian culture. Beyond this, she learned about family planning methods-both the challenges and critical benefits. And as mentioned before, Sarah clearly learned more about herself, her own strengths, her capabilities, and the areas in which she can further improve.
by Sarah Kammerer, 2nd year MCH-MPH student
Preventing Unsafe Abortions in Thailand

Preventing Unsafe Abortions in Thailand
For my practicum, I worked in Thailand with the Women’s Health and Reproductive Rights Foundation (WHRRF) of Thailand, an NGO which works to promote abortion training. The organization advocates for change in the abortion laws, which currently allow for abortion only in the case of risk to maternal physical health or pregnancy resulting from rape.
I began my trip to Thailand by participating in the “Executive Brainstorming Meeting on Modification of Medical Curriculum for Prevention of Unsafe Abortion” organized by WHRRF. This was a meeting of academic physicians from medical schools all over Thailand to discuss the importance of safe abortion trainings for residents and medical students. At the meeting, I gave a lecture about our training in the U.S. and also participated in discussions with the Thai physicians about modifying their current curriculum.
A woman cutting durian in the market
I spent the remainder of my trip speaking with physicians and other health workers about the importance of access to safe abortion services, in many different settings. These settings included a teaching hospital in a southern province, an outpatient abortion clinic in Malaysia, rural hospitals, primary care clinics, STI prevention clinics, the Ministry of Health, and three different academic centers in Bangkok. Through these discussions, I have gained a deeper understanding of the country’s successes and challenges in the fields of contraception and abortion. I was impressed with people’s willingness to speak with me honestly and openly about these controversial issues. Lastly, I was honored to be invited to speak about the importance of safe abortion in many different settings, while in Thailand.
by Britt Lunde, 2nd Year MCH-MPH Student, Family Planning Fellow
Please note that not all practicum experiences are abroad. Many MCHP students work with local organizations on various projects.
A SPACE FOR LEARNING, GROWING, AND FEELING INSPIRED

Posted: October 3rd, 2011
As a volunteer, I had the opportunity to participate in the Maternal and Child Health National Leadership Retreat this summer. The theme was “Leadership, Legacy, and Community” and throughout the three-day retreat, it became very clear how this truly prospers. There was an intentional focus on intergenerational connections, especially in learning from one another in our leadership and practice, discussing the current issues we face in government, in academia, and in the field, and from this, passing down the torch of the maternal and child health profession—with integrity, enthusiasm, and sincere trust.
This was extremely unique and unlike any other conference, workshop, or retreat I had been to before. The theme of community also took shape, not only in the daytime group activities, but in the evening social gatherings. I remember sitting around a small wooden table with key MCH leaders (such as Dr. Arden Handler and Amy Fine) eating refreshments and hearing invigorating stories, over and over, about their past successes in public health policy and even how they happily landed themselves in MCH leadership. This was inspiring to me and also a helpful guide, in knowing that I’m only beginning this journey.
Along with this, the retreat had a focus on building a “Community of Practice” and emphasized collaboration and genuine exchange across the “different lands,” as we called it, within MCH work (i.e. government officials; faculty and staff in academia; students in academia; practitioners in the field). Everyone had something to contribute to the overall community and would help to improve the health and wellbeing of maternal and child health populations, just in a variety of ways.
In conjunction with building a community of practice, there was a particular focus on discussing the life-course perspective throughout the seminars. I think it was valuable to tie in this perspective because we are at a pivotal moment in maternal and child health—with rising health care costs, increasing health disparities, and overwhelming amounts of chronic disease. Through discussions of this perspective, it became obvious that this could help frame our necessity to expand services, adjust programming to critical time periods throughout the life-course, and thus enhance the health potential of communities throughout the U.S. and improve overall health equity.
space continued

One of my favorite lectures during the retreat was by Michael Fraser (Executive Director of the Association of Maternal and Child Health Programs). With humor and charm, he spoke quite clearly about the need for us, as public health leaders, to advocate for MCH populations within our daily work. Especially in a time of budget-cuts and high unemployment, we each have a part to play in the policy-making process. Fraser described advocacy as a combination of education and “urging action.” It wasn’t something scary, overwhelming, or just what the policymakers do. It is within our leadership competencies and our public heath agenda. It requires a deliberate investment with our time, our money, and our voices.
Overall, the retreat was a wonderful experience for me as a graduate student still in training. It helped me to reflect on my own leadership skills and how I can contribute to the overall success and future of maternal and child health field.
by Jessica Barnes, 2nd Year MCH-MPH Student
If you would like to view pictures from the 2011 retreat click here.
TOP TEN LIST: TEN MOST SIGNIFICANT ACHIEVEMENTS IN MATERNAL AND CHILD HEALTH, 2001-2010

Posted: October 3rd, 2011
Number 10
Newborn Screening
Expansion of blood-sample based newborn screening from a handful to more than 29 conditions in almost every state.
Development of universal newborn hearing screening with diagnosis and intervention. This is not a job completely done, but a dramatic change from beginning to end of the decade.
Number 9
Folic Acid-Preventable Neural Tube Defects
Worldwide progress occurred in preventing anencephaly and spina bifida through fortification of food sources with folic acid.
More work remains – experts estimate that 20% are now prevented. Experts differ as to whether additional cases in the US could be prevented with increased levels of folic acid fortification.
Number 8
Mental Health in MCH
The decade brought greater recognition of mental health issues in children. Even more dramatic was the emerging awareness of the importance of maternal mental health, especially perinatal mood disorders and postpartum depression.
Number 7
Child Lead Exposure
The decade saw continued reduction in the proportion of infants and young children with elevated blood lead levels, and intervention programs became more focused through the use of enhanced databases and geographic information systems analyses.
Number 6
MCH Epidemiology
MCH epidemiology was an established field in 2001, but this decade saw it placed firmly in the pantheon of public health, with dedicated MCHEPI positions in almost every state. The annual MCH Epidemiology Conference grew to 500 annual participants, and the annual MCH Epidemiology awards developed considerable prestige.
Number 5
Immunizations
The decade saw the development or implementation of numerous vaccines. Several additions to the required schedule for infants and children have resulted in significant reduction in morbidity (i.e. rotavirus, Hepatitis B), while the pneumococcal vaccine has led to a dramatic decline in invasive pneumococcal infection in young children.
Number 4
Prematurity Prevention
It’s been said that what goes around comes around, and that seems to be true. Although there is increasing recognition of the social determinants of preterm birth, at least, 30-40 years after first being introduced we remembered that progesterone is useful for prevention of some preterm births.
Now if we could only figure out how to offer it as a quality product for a reasonable price . . .
Number 3
Quality Improvement
The decade saw an emerging focus on quality improvement in obstetrics and newborn care, spurred initially by the Vermont-Oxford Network, then by the Joint Commission and ACOG, and more recently AHRQ’s initiation of safety and quality indicators for pregnant women.
There is much more work to be done, including a focus on quality in prenatal care.
Number 2
Universal Access to Prenatal Care?
Okay, we didn’t achieve this, but we did get expanded access to health insurance, especially for infants and children and to some extent for women in pregnancy. We also saw the emergence of new models of care such as Centering Pregnancy. And the Affordable Care Act was passed in 2010, though few of its provisions had been implemented by the end of that year.
Number 1
Well-Woman Care
Beginning in mid-decade, putting preconception and interconception care on the map, and maternal health in general into the framework of well-woman care.
There is still a great deal of work to do, but a promising start occurred in the past decade.
But Just Like Women’s Work, MCH is Never Done…Here’s a partial list of remaining challenges:
- Advancing maternal age
- Limited progress on increasing pregnancy intervals
- Half of all pregnancies are still unplanned
- Few women know about or receive preconception/interconception care
- We’ve made very slow progress on Baby Friendly Hospitals, almost none on the Mother Friendly Hospital initiative
- Data integration is occurring, but the pace is glacial (both in clinical and public health settings)
- Federal and state budget cuts are leading to dismantling of some publicly funded programs
- Malpractice and defensive medicine practices
- Regionalized systems of care losing ground
- High-risk infant follow-up no longer occurs except for lucky infants who enter EI immediately or are enrolled clinical trials
- Public apprehensiveness to child vaccines
- And many more . . .
By Russell Kirby, Ph.D., M.S., Professor, University of South Florida, College of Public Health, Community and Family Health
Dr. Kirby also serves on the UIC MCHP National Retreat Planning Committee.
Inspired by “Ten Great Public Health Achievements—United States, 2001-2010”, MMWR 2011, May 11;60,19: 619-623.
With apologies to David Letterman, and thanks for editorial assistance to Elizabeth Kirby and for their insights to the following contributors:
- Godfrey Oakley, Emory University
- Judith Vessey, Boston College
- Kate Kvale, Wisconsin Department of Health Services
- Mark Walker, University of Ottawa
- Arden Handler, University of Illinois-Chicago
- Lisa Korst, University of Southern California
Click here if you would like to read some of Dr. Kirby’s other Top 10 Lists.